- Home
- About
- Committees
- Finance and Reimbursement
SCEMSA Finance and Reimbursement committee
This committee develops and monitors finance and reimbursement practices and issues that impact EMS systems and providers and works with local, state, and federal partners to improve payment models and allowable funding options.
This page was created to be a resource for those interested in EMS finance and reimbursement. We will post important news, documents, and resources in one place. Some resources may only be available to SCEMSA members only. If you would like to stay informed and get additional benefits, make sure to keep your membership current or join us today!
Below you will find information on the SC Ambulance Supplemental Payment Program with Public Consulting Group. SCEMSA also sent out a RFP this fall for a Provider Assessment Program. We are in the process of awarding that RFP and signing a contract. The goal is to provide funding and reimbursement to all types of EMS agencies - public and private. Stay tuned or join us for an upcoming committee meeting to learn more. Quarterly committee meeting dates and zoom information are located on our events calendar.
If you are interested in joining this committee or others, edit your membership profile by logging into the SCEMSA website in the upper right. Or contact a committee chair via their information on our leadership page.
South Carolina Ambulance Supplemental Payment Program (ASPP) OverviewSouth Carolina EMS Association (SCEMSA) and Public Consulting Group (PCG) have partnered to develop and implement an ambulance supplemental payment program (ASPP) that will provide significant relief to South Carolina’s public ambulance providers.Download the full program overview here. CALL TO ACTION: 3 Ways to Get Involved Today
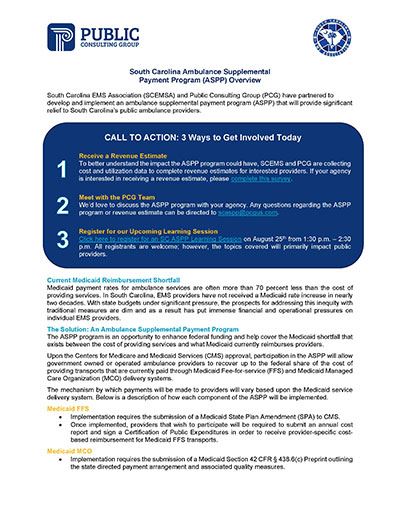
Current Medicaid Reimbursement ShortfallMedicaid payment rates for ambulance services are often more than 70 percent less than the cost of providing services. In South Carolina, EMS providers have not received a Medicaid rate increase in nearly two decades. With state budgets under significant pressure, the prospects for addressing this inequity with traditional measures are dim and as a result has put immense financial and operational pressures on individual EMS providers. The Solution: An Ambulance Supplemental Payment ProgramThe ASPP program is an opportunity to enhance federal funding and help cover the Medicaid shortfall that exists between the cost of providing services and what Medicaid currently reimburses providers. Upon the Centers for Medicare and Medicaid Services (CMS) approval, participation in the ASPP will allow government owned or operated ambulance providers to recover up to the federal share of the cost of providing transports that are currently paid through Medicaid Fee-for-service (FFS) and Medicaid Managed Care Organization (MCO) delivery systems. The mechanism by which payments will be made to providers will vary based upon the Medicaid servicedelivery system. Below is a description of how each component of the ASPP will be implemented. Medicaid FFS
Medicaid MCO
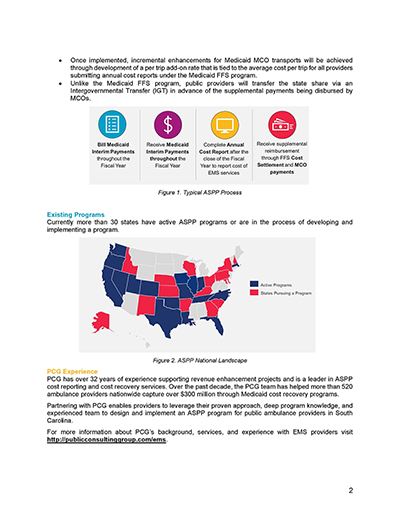
Existing Programs Currently more than 30 states have active ASPP programs or are in the process of developing andimplementing a program. PCG ExperiencePCG has over 32 years of experience supporting revenue enhancement projects and is a leader in ASPP cost reporting and cost recovery services. Over the past decade, the PCG team has helped more than 520 ambulance providers nationwide capture over $300 million through Medicaid cost recovery programs. Partnering with PCG enables providers to leverage their proven approach, deep program knowledge, and experienced team to design and implement an ASPP program for public ambulance providers in South Carolina.For more information about PCG’s background, services, and experience with EMS providers visit http://publicconsultinggroup.com/ems. |